What is Hip Replacement Revision Surgery?
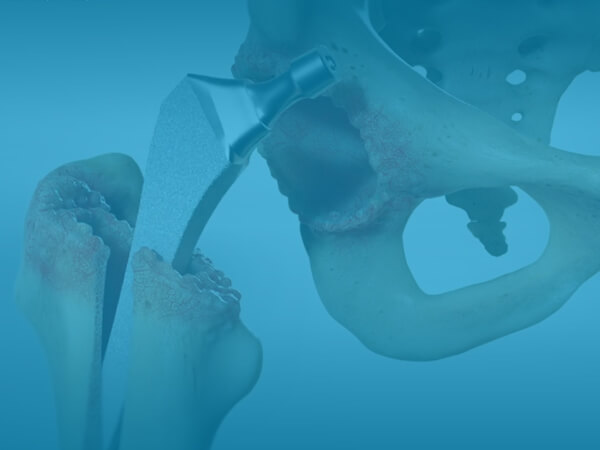
During this surgery, a surgeon removes some or all parts of the old ball and socket joint implant and replaces them with new implants. Different implants with longer and thicker stems in the thigh bone are often required to stabilize the new joint and achieve a similar level of support and range of motion. In rare cases where there has been significant bone loss, the surgeon may address that as well with a combination of bone grafts, wires or screws to strengthen the bone.
Who should have a Hip Replacement Revision Surgery?
- Someone whose original implant has become loose from the bone. Maintenance of an active lifestyle, increased body weight, or a fracture due to trauma or poor bone quality can result in loosening of the implant.
- Someone whose implant has reached the end of its useful life (usually 15-30 years) and is ‘worn out’. This is caused over time by friction of the implant parts.
- Someone whose original implant has become infected. This can happen even years after the first hip replacement surgery. This is the leading cause of revision, so OrthoNebraska takes extra care during the first surgery to avoid infection.
- Someone whose joint has become too stiff for them to tolerate due to excessive scar tissue built around the hip joint.
Does a Hip Replacement Revision Surgery work?
More than 90 percent of patients should expect good to excellent results, meaning significant pain relief, stability and function of the affected hip joint. Mild pain can sometimes persist after surgery. In rarer cases, pain will always be an issue. Fortunately, in most cases, over-the-counter pain medications can usually treat the remaining level of pain.
Revision surgery is complicated, and thus has slightly higher risks of typical surgical complications such as blood clots, infection or anesthesia problems than an original hip replacement. There is also an increased risk for hip dislocation after revision surgery. At OrthoNebraska our surgeons work diligently with the therapy staff to ensure proper precautions and gait training is taught during the postoperative period to help avoid hip dislocation.
What can I expect when I get a Hip Replacement Revision Surgery?
After your surgery is scheduled at OrthoNebraska Hospital, a nurse navigator will reach out to you to discuss your needs and encourage you to review our online educational videos and guide to help you prepare.
Some example of things we will encourage you to do:
- Plan on having some help at home for the first few weeks after your procedure. Although you may be functionally independent a bit sooner, you will likely tire easy and want at least some help.
- Plan ahead at home and think about ways to make maneuvering around your house and kitchen easier, clearing obstacles out of the way, and removing large rugs.
- Make sure all handrails are secure and that loose cords are tucked away to prevent falling.
You will need a pre-surgical physical from your primary care doctor and possibly other specialists such as Cardiology and/ or Pulmonology to ensure you are healthy for hip replacement revision surgery at OrthoNebraska. After you check in at the hospital on the day of surgery, you will speak with your physician and anesthesiologist before surgery. The anesthesia team will discuss the various levels of sleep you might be appropriate for based on your individual needs, which may include a nerve block, spinal, or general anesthesia. Your surgery will likely take approximately 2-3 hours. Following surgery, you will be in the recovery room for another 1-2 hours before going upstairs to your private room.
Once you are settled in your room, your therapy team and nurse navigators will work with you and your doctor to monitor your progress toward independence with your discharge goals. While this is highly individual, many patients are able to discharge back to home the next day. Whether you are going home with help or alone, you can feel confident that your discharge plan is safe for you.
Recovery after a revision surgery is often unpredictable and varies significantly from patient to patient. You will feel mostly back to ‘normal’ after eight to twelves weeks. Full recovery may take about a year, dependent on your general health and dedication to measured progress in therapy.